Could your heart be harboring hidden vulnerabilities that only surface under stress—threatening your health silently? Cardio stress tests serve as a crucial window into your heart’s true resilience, revealing issues like blocked arteries or electrical irregularities that might go unnoticed during rest. This controlled exertion mimics real-world activity, helping doctors detect early warning signs before symptoms appear or damage occurs. As technology advances, these tests are becoming more accurate and accessible, empowering proactive prevention rather than reactive treatment. Imagine catching silent risks early enough to prevent a heart attack or long-term damage—doesn’t that urgency highlight the importance of regular screening, especially if risk factors run in your family? In a world moving toward personalized heart care, understanding and acting on these insights can mean the difference between a life of health and one shadowed by unseen danger. Are you ready to take control of your heart’s future?
Unlocking Heart Secrets: The Power of Cardio Stress Tests
A cardio stress test is a straightforward yet powerful tool that helps doctors see how your heart performs during physical activity. Instead of just measuring your heart at rest, this test pushes it a little harder—usually by walking on a treadmill or pedaling a stationary bike—while your vital signs are monitored closely. It’s like giving your heart a gentle workout in a controlled setting to observe how well it handles exertion.
The main goal is to uncover hidden issues that might not show up when your body is at rest. Many heart problems, such as narrowed arteries or electrical irregularities, only become apparent when the heart is working harder. During a stress test, changes in your ECG, blood pressure, or symptoms like chest pain can signal potential trouble, even if you feel fine otherwise.
This assessment is especially valuable for those with risk factors like high blood pressure, high cholesterol, or a family history of heart disease. It’s also often recommended if you experience symptoms like shortness of breath or chest discomfort during activity. By simulating physical stress, the test reveals vulnerabilities that are otherwise difficult to detect, providing a clearer picture of your heart’s health.
The procedure itself lasts about 15 to 30 minutes. You’ll begin walking or cycling at a gentle pace, with the intensity gradually increasing. Throughout, sensors track your heart’s electrical activity, blood pressure, and breathing. Sometimes, imaging techniques are added to get a more detailed view of blood flow and heart function, making the test even more informative.
Preparing for a stress test is simple—wear comfortable clothing, avoid caffeine, and don’t eat a heavy meal beforehand. The process is non-invasive and safe, with medical staff closely monitoring your response at all times. Their goal is to ensure your safety while gathering accurate data on how your heart responds under stress.
Understanding what a stress test involves can help ease any concerns. It’s a routine procedure designed to provide vital insights into your heart’s resilience. In many cases, the test uncovers issues that are silent but potentially serious, giving you and your doctor a head start on managing your heart health.
Ultimately, a cardio stress test serves as a window into your heart’s true performance—highlighting strengths and revealing vulnerabilities. It’s a key step in catching problems early, guiding treatment, and helping you make informed decisions about your activity and lifestyle. Knowing and acting on these insights can make a significant difference in maintaining a healthy, active life.
Heart Fundamentals: Anatomy, Diseases, and Risks
The heart is a muscular organ roughly the size of a fist, tirelessly pumping blood to sustain your body. It’s divided into four chambers: two upper atria and two lower ventricles. These chambers work in sync, with electrical signals orchestrating each heartbeat to ensure blood is propelled efficiently through your arteries and veins. When functioning normally, your heart operates quietly and without fuss, quietly supporting your every move.
However, problems can develop without obvious warning. One of the most common issues is coronary artery disease, where arteries supplying blood to the heart become narrowed or blocked by plaque buildup. This can lead to symptoms like chest pain, shortness of breath, or, in severe cases, a heart attack. Electrical disturbances, known as arrhythmias, cause irregular heartbeats that may be too fast, too slow, or erratic, potentially leading to dizziness or fainting. Heart failure occurs when the heart’s pumping ability weakens, making it harder to meet your body’s oxygen and nutrient needs.
Many risk factors contribute to heart problems. Unhealthy lifestyle choices—such as smoking, poor diet, physical inactivity, and excessive alcohol consumption—play a significant role. High blood pressure, elevated cholesterol, and diabetes further increase vulnerability by damaging blood vessels or impairing heart function. Family history can also predispose individuals to inherited conditions. Stress and poor sleep might seem unrelated but can gradually weaken heart health over time, emphasizing the importance of holistic lifestyle management.
In the past, diagnosing heart issues relied heavily on physical exams and listening to heart sounds. The introduction of electrocardiograms revolutionized detection by recording electrical activity, helping identify arrhythmias and ischemia. Today, advanced tools like stress testing, echocardiography, and nuclear scans provide detailed insights into both the structure and function of the heart, enabling earlier and more precise intervention.
Understanding these fundamentals of heart health highlights why early detection matters. Many silent conditions, such as narrowing arteries or electrical irregularities, often remain unnoticed until they cause serious problems. Recognizing risk factors and knowing how the heart works empowers you to take proactive steps—whether through lifestyle changes or medical screenings—to protect your heart now and in the future.
Revealing Hidden Heart Weaknesses Through Stress Testing
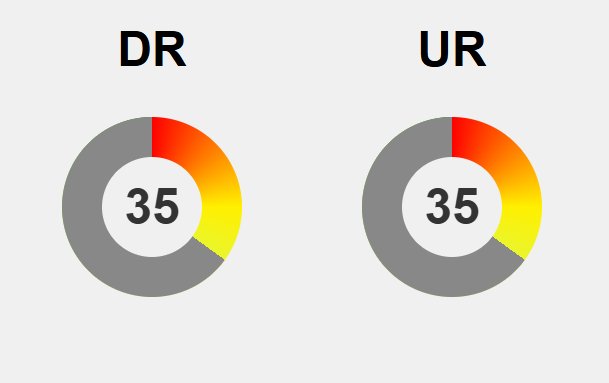
When your heart is pushed during a stress test, it can reveal vulnerabilities that often stay hidden during normal activity or rest. Many issues, like narrowed arteries or electrical disturbances, only become apparent when the heart is working harder. For example, reduced blood flow—known as ischemia—might cause chest pain or ECG changes during exertion, serving as an early warning sign that parts of the heart aren’t receiving enough oxygen. These signals often appear before any symptoms do, giving doctors a crucial window to intervene early.
Research consistently shows that abnormal findings during stress testing are strong predictors of future heart problems. When the heart struggles to meet increased demands, it can produce abnormal ECG changes or irregular rhythms. These clues point to underlying issues like blocked arteries that might not cause trouble at rest but become problematic under stress. Detecting such issues early allows for timely treatment, reducing the risk of heart attacks or other serious events down the line.
Stress tests are also valuable for uncovering electrical problems like arrhythmias that don’t show up during routine exams. Irregular heart rhythms often only surface when the heart is under strain, making their detection vital. Identifying these electrical disturbances helps doctors assess the heart’s electrical stability and plan appropriate therapies, whether medications or device interventions. This comprehensive view ensures that both structural and electrical vulnerabilities are addressed before they cause emergencies.
However, no diagnostic method is infallible. False positives can lead to unnecessary worry or additional testing, while false negatives might create a false sense of security. Factors like patient effort, medication use, or technical limitations can influence results. For instance, some individuals may not reach their target heart rate due to age or physical ability, potentially skewing the outcome. Recognizing these limitations helps ensure stress test results are interpreted within a broader clinical context.
Interpreting the results requires nuance. Signs of ischemia or abnormal rhythms indicate areas where blood flow or electrical activity may be compromised, but they don’t always spell immediate danger. Some findings can be benign or require further confirmation, while a normal test doesn’t guarantee immunity from future issues, especially if risk factors persist. Combining stress test data with other clinical information provides a fuller picture of heart health, guiding more accurate decisions.
In essence, stress tests amplify the signals from your heart, exposing weaknesses that often go unnoticed. By mimicking physical exertion in a controlled environment, they reveal how well your heart responds under stress. This insight is vital for catching problems early—before symptoms appear or damage occurs—allowing for targeted interventions that can improve long-term outcomes. Detecting these hidden vulnerabilities is a key step in preventing serious heart events and maintaining your heart’s resilience.
Understanding these potential issues underscores the importance of comprehensive heart evaluations. For those interested in learning more about how stress testing can identify hidden heart issues, exploring additional resources like stress testing benefits can provide valuable insights. Staying informed helps you make proactive decisions for your heart health.
From Detection to Action: How Stress Tests Shape Heart Care
When a stress test uncovers signs of reduced blood flow or electrical instability, it often prompts early, targeted interventions. These might include lifestyle modifications like adopting a healthier diet, increasing physical activity, or quitting smoking. Medications such as statins or blood pressure reducers can be prescribed to manage underlying risks before they lead to serious damage. In some cases, the findings may lead to further procedures, like angiograms, to pinpoint and treat blockages more precisely. Acting on these early signals can prevent the progression of disease and significantly lower the chances of a heart attack or other emergencies.
Detecting issues through stress testing allows for a personalized approach to treatment. For example, if a test reveals significant artery narrowing, procedures like angioplasty or stenting might be recommended to restore blood flow. Conversely, if electrical irregularities are identified, medications or devices can be used to stabilize the heart rhythm. This tailored strategy reduces the likelihood of future crises and improves long-term outcomes, ensuring interventions are appropriate and effective for each individual.
Stress test results also serve as a powerful motivation for healthier habits. When the test highlights early signs of vulnerability, many people become more committed to heart-healthy choices like balanced eating, regular exercise, and stress management. These lifestyle changes often lead to a decreased need for medications or invasive procedures, emphasizing prevention over reaction. The test acts as a wake-up call, inspiring action that can ultimately protect your heart and improve overall well-being.
For healthcare providers, stress testing offers valuable insight into a patient’s risk profile. It helps determine who would benefit from more aggressive treatments and who can safely continue with conservative management. This targeted approach prevents unnecessary procedures for low-risk patients while ensuring high-risk individuals receive the care they need. Using stress test outcomes in this way makes treatment more precise and efficient, optimizing outcomes and resource use.
While there are challenges related to access and cost, the benefits of early detection are clear. Catching silent risks before they cause symptoms saves lives and reduces long-term healthcare costs. As new technologies emerge—like portable devices and AI-driven analysis—the ability to identify vulnerabilities earlier and more accurately will only improve. Expanding access to these tools can shift the focus from reactive care to proactive prevention, making a real difference in public heart health.
The future of heart care is moving toward more personalized, preventive strategies. Wearables and continuous monitoring devices, combined with advanced data analysis, will enable real-time risk assessment and early intervention. This shift allows for tailored treatment plans that adapt to your changing health status, reducing the likelihood of severe events. By prioritizing prevention and early detection, we can help more people maintain healthy, resilient hearts well into the future.
In the end, stress testing’s role extends beyond diagnosis—it becomes a catalyst for action. Early insights gained from these assessments empower individuals and doctors to address vulnerabilities before they escalate into emergencies. This proactive approach not only saves lives but also fosters a mindset of ongoing care and prevention. Embracing these tools and strategies means taking control of your heart health today, for a healthier, longer tomorrow.
The Future of Heart Health: Innovations, Insights, and Prevention
Advancements in heart health detection are opening exciting new pathways for early intervention and prevention. Technologies like AI-powered imaging, wearable monitors, and portable stress testing devices are making assessments more accurate, accessible, and real-time. These innovations enable us to spot hidden risks long before symptoms appear, shifting the focus from reactive care to proactive management. As research accelerates, efforts to lower costs and expand availability are crucial to ensuring everyone benefits from these breakthroughs.
Early detection through stress testing has proven to be a game-changer. By revealing vulnerabilities like blocked arteries or electrical irregularities early on, these tests provide a crucial window for action. Catching issues before they cause symptoms means treatments can be more effective, whether through lifestyle changes, medications, or further diagnostics. This shift toward prevention reduces the incidence of severe heart events and helps people maintain healthier, longer lives.
Emerging tools like AI analysis enhance our ability to interpret complex data quickly and with high precision. Wearables are evolving to monitor heart activity continuously, offering ongoing insights that can detect problems in real time. Portable stress testing devices are on the horizon, promising to bring assessments outside traditional clinics into everyday settings. These trends point toward a future where heart health monitoring becomes an integral part of daily life, empowering individuals to stay ahead of silent risks.
For individuals, staying informed and proactive is more important than ever. Regular check-ups, especially if you have risk factors, can now include advanced screenings that identify subtle signs of trouble early. Discussing options like stress testing with your healthcare provider can help you understand your personal risk profile and take preventive steps. Instead of waiting for symptoms to appear, you can act early—saving yourself from potential crises and supporting lifelong heart resilience.
However, challenges such as ensuring equitable access and affordability remain. Bridging the gap between technological innovation and widespread availability is vital to reduce disparities in heart health outcomes. As technology advances, making these tools affordable and user-friendly will be key to reaching underserved populations. Expanding access can lead to a significant reduction in silent heart risks across diverse communities, ultimately saving more lives.
Looking ahead, the integration of these cutting-edge tools promises a future where heart disease prevention is more personalized and dynamic. Continuous monitoring devices combined with AI-driven insights will enable tailored interventions that adapt to your changing health needs. This proactive, data-driven approach can drastically decrease the occurrence of severe heart events, fostering a society where healthier hearts are the norm rather than the exception.
Focusing on early detection and prevention transforms how we approach heart health. Instead of waiting for warning signs or emergencies, we can now identify vulnerabilities long before they manifest as symptoms. This shift not only saves lives but also encourages a mindset of ongoing care, empowering individuals to take control of their well-being. Embracing these innovations paves the way for a future where resilient hearts and healthier communities become the standard.